Sleep Deprivation Among Frontline Health Care Workers During COVID-19 Turns Critical
The pandemic's impact stretches across all aspects of life, and has particularly concerning effects on the sleep of those working on the frontlines providing care of patients.
Michael Grandner, PhD, MTR, CBSM, FAASM

As a year of unchecked surges of coronavirus disease 2019 (COVID-19) infection comes to a close, sleep deprivation among health care professionals (HCPs) has become a major concern. Are they functioning well enough at work? Are they showing other signs of stress outside the hospital? Several reviews and surveys have attempted to evaluate and quantify the effects of these unrelenting stressors on the mental and physical health of HCPs treating patients with COVID-19.1,2
A Problem of Unprecedented Magnitude
The impact of the pandemic and subsequent lockdowns on sleep has been universal, according to Michael Grandner, PhD, MTR, CBSM, FAASM, director of the Sleep and Health Research Program and the Behavioral Sleep Medicine Clinic at the University of Arizona College of Medicine in Tucson. In an interview with NeurologyLive, he said, “There is not 1 person anywhere whose sleep has not been affected at all by the pandemic. It’s a foundation of our biology. Paradoxically, everyone’s sleep is affected differently.”
Lack of sleep among HCPs is now a critical problem, as they struggle to cope with the personal aspects of COVID-19 while treating those who become sick. A meta-analysis of 53 studies reported a pooled prevalence of poor sleep quality in up to 61% of nurses in general,1 whereas a 2020 survey in China showed that more than one-third of all medical staff there experienced symptoms of insomnia associated with the COVID-19 pandemic.2
William D. Killgore, PhD

“Health care workers, in particular, have had to work long hours with limited resources and in close proximity to COVID-19 patients during the pandemic,” William D. Killgore, PhD, director of the Social, Cognitive, and Affective Neuroscience (SCAN) Lab in the Department of Psychiatry at the University of Arizona, told NeurologyLive. The SCAN Lab uses advanced technologies to map neurological processes and responses. “As the hospitalization rates continue to surge again, many health care workers are experiencing high levels of stress, anxiety, depression, burnout, and insomnia,” he said.
Sleep Domains Affected
Sleep parameters affected by the pandemic include sleep latency, duration, and efficiency.3 Some studies suggest that insomnia, or difficulty falling asleep or remaining asleep, is reported by more than half of health care workers who work with patients with COVID-19, Killgore said. “Many health care workers are showing signs of posttraumatic stress, which is often associated with nightmares and disturbed sleep. Unfortunately, sleep is important for the ability to process through emotional experiences, so the sleep disruption due to anxiety, long hours, and stress can lead to a vicious circle that maintains sleep problems and the emotional effects of traumatic experiences.”
Mechanisms of Sleep Deprivation in HCPs
HCPs on the front lines experience greater sleep deprivation as a result of increased sleep restriction from extended work schedules, coupled with various insomnias once they return home. Jessica Dietch, PhD, of the Department of Psychiatry and Behavioral Sciences at Stanford University School of Medicine in California, explained that prior to the pandemic, shift work, particularly that involving rotating shifts, was associated with worse sleep across the domains (latency, duration, and efficiency), which were exacerbated with the changing shift demands that occurred once COVID-19 hot spots were apparent.
Jessica Dietch, PhD

Additional stressors have included extreme variability to sleep duration along with increased work and family demands, each of which may limit sleep opportunities for HCPs by restricting the average amount of sleep to less than needed. “Decreased sleep duration, particularly that occurring over multiple days or weeks in a row, can lead to the accumulation of sleep debt,” Dietch told NeurologyLive. “Additionally, we know that increases in stressors, which abound for HCPs during the COVID-19 pandemic, can precipitate new insomnia, such as difficulty falling or staying asleep, or exacerbate existing insomnia,” she said.
“Insomnia occurs when there is a decreased ability to detach at night,” Grandner added. This causes sleep to become more fragmented and more shallow, although he noted that in laboratory studies, impairments after a night or 2 of sleep deprivation tend to be less than expected. “Impairments accumulate after a few days or nights of sleep deprivation,” he explained. “Your body will entrain arousal when you’re up night after night, leading to a pattern of chronic insomnia.”
The neurologic impact after loss of sleep over multiple nights is significant. According to Killgore, lack of sleep leads to a reduction of metabolic activity in regions of the brain that are critical for attention, decision-making, and emotional regulation. “Sleep loss has been associated with reduced functional connectivity, ie, communication, between the emotional regions of the brain and the regions that normally regulate those areas, potentially leading to an increased tendency to view experiences from an emotionally skewed, usually negative, perspective,” he said.
Altered Cognition
Sleep deficits begin to lead to pronounced alterations of cognition, Killgore said, with potentially serious consequences. “When a person is lacking restorative sleep, they build up a biological ‘pressure’ to fall asleep, which eventually starts to intrude upon their waking performance in the form of brief attentional lapses. These are momentary glitches, often less than a second in duration, in ongoing cognitive processing where mental activity just seems to stop for a moment. The problem is that these lapses are uncontrollable and occur without warning,” he said, while driving or working, for instance. Consequently, these lapses can be life-threatening.
The most significant impacts on job performance show up not as much in routine, repetitive tasks, according to Grandner, but “when someone has to make a novel judgment call, like when driving home and the light changes or an animal darts into the road.” Such loss of judgment or decision-making abilities resulting from cognitive slowing, in which processing critical information and solving problems take longer, represents potentially the most catastrophic effect of continued sleep loss. Killgore explained that “a sleep-deprived health care provider may not see a simple solution to a simple problem that just takes a different perspective. It also affects judgment and willingness to take risks and how they make moral decisions. So a health care worker who is lacking sleep may make very different life-or-death decisions than they would if they were well-rested.”
Health care workers who do shift work—ie, working at times that are biologically out of alignment with their normal day-night rhythm—also seem to be at greater risk for insomnia and other psychological problems during the pandemic.— WILLIAM D. KILLGORE, PHD
Disordered Emotional Processing
A tired baby is a cranky baby, and the same is true for adults, although at work, they may try to hide it. Sleep deprivation alters mood and emotional processing as well as alertness. Without sufficient sleep, individuals are prone to emotional and physical burnout, and normally manageable tasks can easily become overwhelming.
Killgore and his colleagues also found that lack of sleep leads to an increase in implicit biases, such as those against individuals of different races or ethnicities.4 “In our study, when sleep was restricted to 4 hours per night for 3 weeks, implicit biases against Arab Muslims were high, but when the same people got 8 hours of sleep a night for 3 weeks, these biases against others completely disappeared,” he said.
Loneliness is a unique and damaging effect of the ongoing pandemic among HCPs, who are away from their families for longer-than-usual periods and who often have to avoid close contact with those they love because of heightened exposure to the virus at work. “Our data show that as the pandemic has raged on, the levels of loneliness and lack of social support among those under lockdown restrictions have been much worse than those in open communities. We have found that those under lock-
down report greater loneliness, depression, anxiety, alcohol abuse, and suicidal thinking than those not under restrictions,” Killgore reported. Lack of sleep has been associated with poor memory and difficulty with attention and concentration. Although causality has not been demonstrated conclusively, nearly every major psychiatric disorder is associated with sleep problems, he said. Killgore noted that some studies have suggested that the emotional toll of the pandemic has been greater on women than men in terms of anxiety and depression. “Health care workers who do shift work—ie, working at times that are biologically out of alignment with their normal day-night rhythm—also seem to be at greater risk for insomnia and other psychological problems during the pandemic,” he added.
Associated Health Risks
Long-term sleep restriction can have many adverse health effects, Killgore explained. “Most notably, long-term insufficient sleep is associated with increased metabolic disturbances, weight gain, obesity, hypertension, diabetes, and greater risk of heart attacks and stroke, as well as weakened immune function,” he said. Not surprisingly, continued sleep deprivation also presents a higher risk of acquiring COVID-19.
“There’s also a potential indirect pathway, in that poor sleep can exacerbate conditions that may be associated with increased risk of infection or complications from COVID- 19, like cardiovascular disease,” Dietch said. “Good sleep health is important to support physical and mental health broadly during the COVID-19 pandemic, although it can be hard to come by for HCPs.”
“Lack of sleep leads to worse mood in healthy people, and sleep is critical for processing through emotions and gaining perspective, so there is strong evidence to suggest that chronic sleep restriction can contribute to greater risk for mental health problems,” Killgore suggested. “Our own research has shown that getting more and better quality sleep is associated with greater resilience during the COVID-19 pandemic.”6
Recognizing When Tired Becomes Too Tired
Killgore pointed out that a sleep-deprived individual who is normally very wise and judicious will not realize when they are sleepy and are making mistakes. Many individuals with chronic sleep problems can get extremely tired and may even fall asleep frequently throughout the day without knowing. He suggested that it is important to take any errors in performance, even minor ones, as serious indicators of impairment. “The best option is to simply follow the science and assume that if you are sleep-restricted, you are probably impaired without knowing it,” he said. “Most people will start to show performance deficits after they have been awake longer than 18 hours straight. Performance declines rapidly over-night from about 11 PM to about 8 AM the following morning.” He suggested that individuals probably show impairment if they are awake at a time when they would normally be sleeping. Chronic sleep restriction down to even 6 hours a night for 2 weeks is nearly equally as impairing as a single night without any sleep, he said, encouraging HCPs to “take it seriously if [they] are dozing off or making simple mistakes at times when [they] should be awake and alert. These are clear signs that [they] are not getting enough sleep.”
Grandner observed that paradoxically, “one of the best clues to impairment is the feeling that you’re starting to adjust to the stress” or the recognition of a heightened emotional status— feeling unusually annoyed, sad, or anxious, for instance. “Feeling indecisive or defensive about decisions [is another sign] that you may be sleep impaired,” he added.
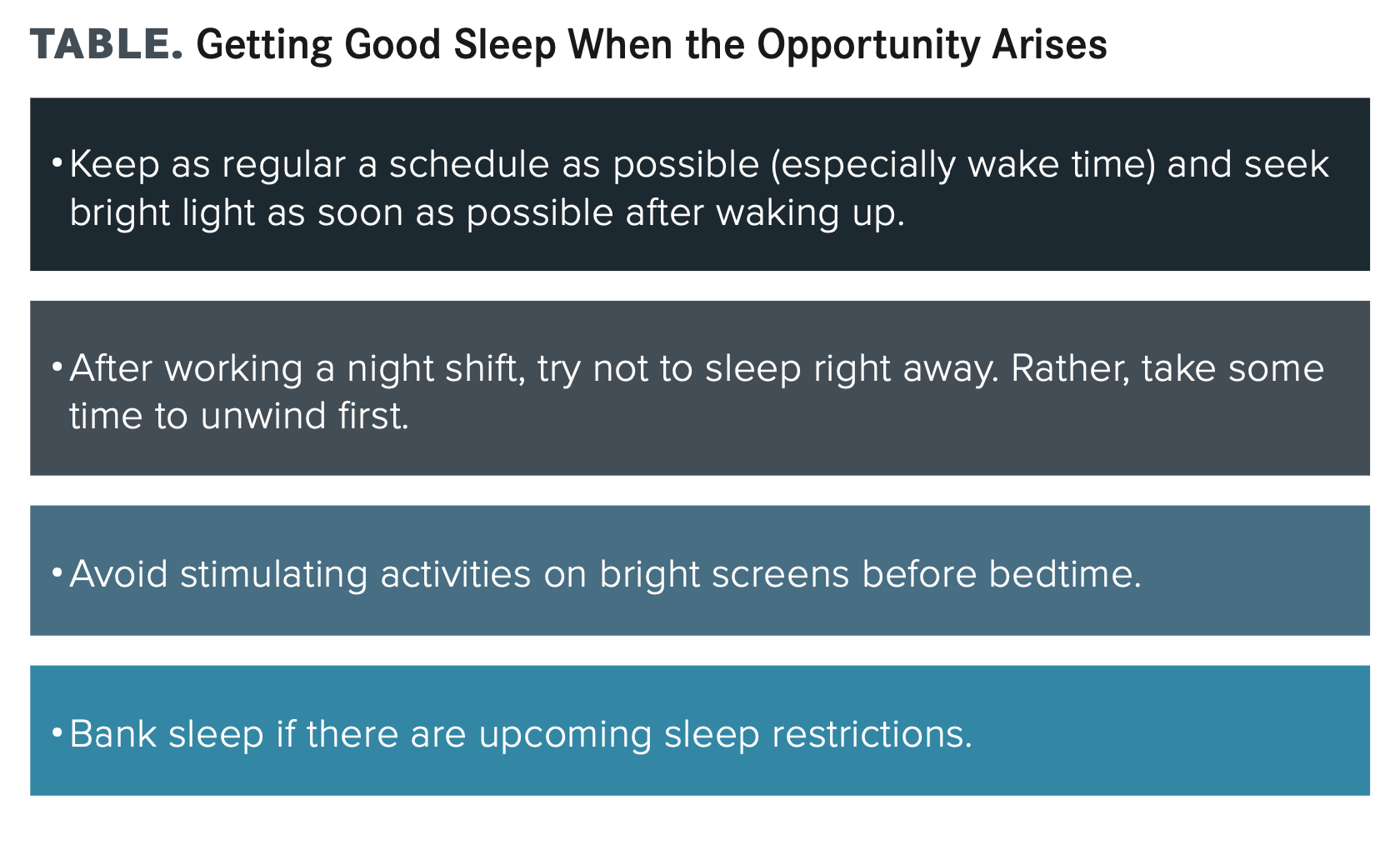
“Unfortunately,” Killgore stated, “there is no substitute for sleep. Sleep is an absolute need, and the body will start grabbing it wherever it can, even at the most inopportune moments, if you are not getting enough. The solution isn’t to swing the pendulum in the other direction—it’s to find balance,” Grandner counseled. He suggested that one of the most important things to do after work is to try to disengage from the day.
Caffeine as a Solution
When sleepiness sets in, individuals can employ a few strategies to remain more alert in the short term, at least until they can catch up on sleep. All the experts agreed that in the short term, caffeine can be very helpful to maintain alertness but that individuals should use it judiciously, as it remains in the body and can cause sleeplessness even 6 to 12 hours after ingestion. “Although caffeine is very effective at sustaining immediate alertness and vigilance performance, it often produces no measurable improvements in judgment and decision-making quality,” Killgore said.
Grandner agreed, adding that “stimulants, including caffeine, all improve fatigue, reaction time, and alertness but do not rescue decision-making. People just make bad decisions faster,” he said.
Maintaining Alertness on the Job
The experts recommended a number of strategies for improving performance and/or wakefulness while at work:
- Take a short walk and seek bright light to promote alertness.
- Consume caffeine early in a shift and cut it off at least 6 to 8 hours before bedtime.
- Eat a snack rather than a large meal during a shift to help promote alertness.
- Schedule small naps in the middle of the day to keep balanced (no more than 15-30 minutes for optimum alertness).
REFERENCES
1. Zeng LN, Yang Y, Wang C, et al. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behav Sleep Med. 2020;18(6):746-759. doi:10.1080/15402002.2019.1677233
2. Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. doi:10.3389/fpsyt.2020.00306
3. Ferini-Strambi L, Salsone M. COVID-19 and neurological disorders: are neurodegenerative or neuroimmunological diseases more vulnerable? J Neurol. Published online July 21, 2020. doi:10.1007/s00415-020-10070-8
4. Alkozei A, Killgore WDS, Smith R, et al. Chronic sleep restriction increases negative implicit attitudes toward Arab Muslims. Sci Rep. 2017;7(1):4285. doi:10.1038/s41598-017-04585-w
5. Killgore WDS, Cloonan SA, Taylor EC, Lucas DA, Dailey NS. Loneliness during the first half-year of COVID-19 lockdowns. Psychiatry Res. 2020;294:113551. doi:10.1016/j.psychres.2020.113551
6. Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020;291:113216. doi:10.1016/j.psychres.2020.113216