4 Advances in Alzheimer
A new way to treat dementia and other diagnosis and treatment developments are in the news.
“©BMCL/Shutterstock.com”
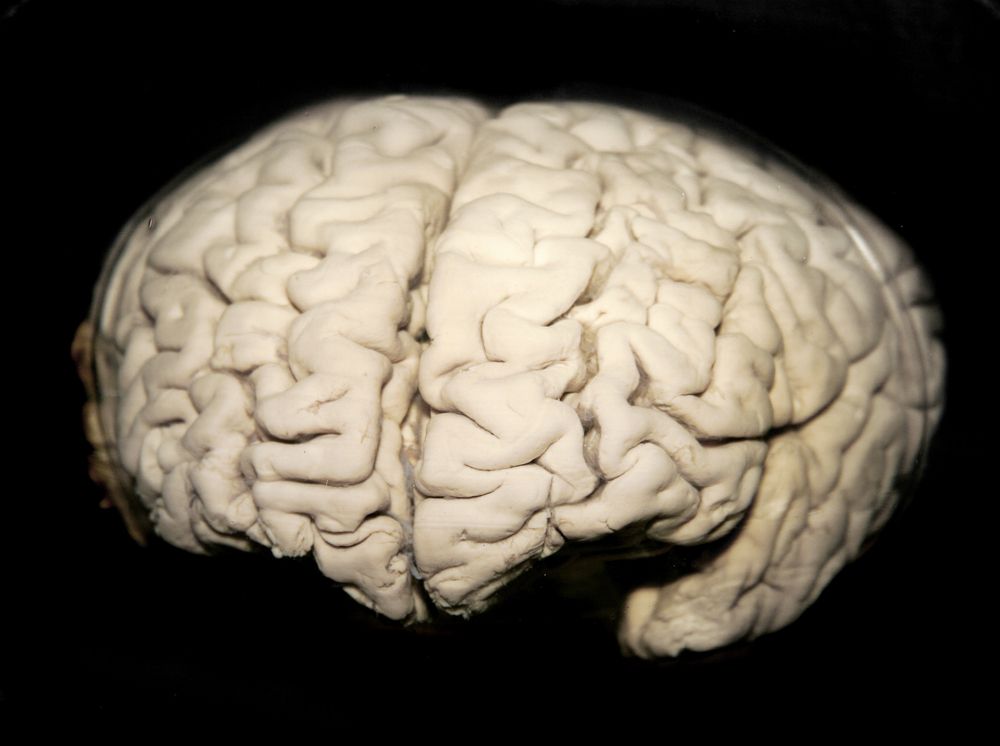
Tau is the major driver of cognitive decline and memory loss in Alzheimer disease (AD); the first clinical trial to identify and treat patients in early AD is under way; a new drug reduces amyloid plaque in AD brains, a new way to treat patients with dementia-these are the most recent advances in AD diagnosis and treatment.
Turn the pages to find out more:
Major Culprit in AD: Tau or Beta-amyloid?
• Debate about whether beta-amyloid or tau drives AD has been raging for decades.
• A new study of more than 3600 postmortem brains conducted at the Mayo Clinic in Florida and Minnesota suggests that tau is the major driver of cognitive decline and memory loss in AD.
• By studying brains at different stages of AD severity, the researchers were able to tell that tau accumulates first.
• The scientists also compared amyloid and tau accumulation with brain scans taken before death.
• The findings offer valuable new information, including the suggestion that tau should be the major therapeutic target of anti-AD drugs.
Identify, Treat Patients in Early AD, Before Memory Loss
• Researchers at Harvard are screening healthy brains for toxic tau.
• The efforts are part of a large clinical trial, Anti-Amyloid Treatment in Asymptomatic Alzheimer’s, or A4.
• Tau often is found in small amounts in healthy persons older than 70 years but generally is confined to the medial temporal lobe, said Dr Reisa Sperling of Massachusetts General Hospital in Boston, who leads the 1000-patient trial.
• Patients in the trial will already have evidence of amyloid buildup and will receive the drug solanezumab or placebo for 3 years.
• This is the first clinical trial to identify and treat patients in early AD, before memory loss.
AD Med May Stop, Even Reverse AD Damage
• A new drug that reduces amyloid plaque in AD brains, aducanumab, has been developed by Biogen.
• PRIME, a study of 166 patients with mild AD, has indicated that the beta amyloid is being removed.
• Patients receiving the drug also have less decline in mental ability, according to the results of a mental acuity test.
• Biogen plans a 1000-patient study based on the success of the medication so far.
Treat Memory Loss from Dementia-related Conditions
• A new way to treat patients with dementia-by sending electrical impulses to specific areas of the brain to enhance the growth of new brain cells-was found by scientists at Nanyang Technological University, Singapore.
• Deep brain stimulation, already used in some parts of the world to treat neurological conditions, such as tremors and dystonia, also could be used to enhance the growth of brain cells, which mitigates the harmful effects of dementia-related conditions and improves short- and long-term memory.
• New brain cells can be formed by stimulating the front part of the brain using minute amounts of electricity.
• The increase in brain cells reduces anxiety and depression, promotes improved learning, and boosts overall memory formation and retention.
• The research findings open new opportunities for developing novel treatments for patients who experience memory loss resulting from dementia-related conditions, such as AD and Parkinson disease.
• The discovery was published in eLife, a peer-reviewed open-access scientific journal.
Take-aways:
• Tau is the major driver of AD and should be the major therapeutic target of anti-AD drugs, suggests a new Mayo Clinic study.
• Anti-Amyloid Treatment in Asymptomatic Alzheimer’s, or A4, is the first study to identify and treat patients in early AD, before memory loss.
• The drug aducanumab has been successful at removing brain amyloid in mild AD and preventing cognitive decline. Researchers are planning a large-scale study.
• Sending electrical impulses to specific areas of the brain to enhance the growth of new brain cells may present a new way to treat patients with dementia.